We have two sets of teeth. Primary dentition consists of 20 teeth and secondary or permanent dentition 32 teeth. The roots of primary teeth will usually dissolve or resorb between the age of 6 to 14, to allow these teeth to drop off and new teeth to come up.
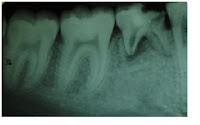
I have encountered cases where the patients have congenitally missing teeth. The medical term for this condition is called 'hypodontia'. The common teeth that are missing in the permanent dentition are upper lateral incisors and lower second premolars. Sometimes their primary/deciduous teeth still remain in the jaws. The patient usually is not aware that the tooth has not been replaced by a permanent one, unless being told by his or her dentist during a routine check-up. I usually confirmed this occurence by taking a radiograph.
There are also cases where the patients complain of toothache due to large decay on these teeth. Sometimes, I perform a root canal treament, provided the root are not resorbed, in order to keep the tooth functioning in the oral cavity for as long as possible, especially for a young patient. However, the prognosis maybe be guarded. It is also possible that the retained primary tooth is fused to the jaw bone (ankylosed). I supposed one will just have to accept the fact that he or she is born with less teeth and ultimately, will need dental implants.

