
A dentist shares her observations and experiences in her daily clinical practice in Petaling Jaya, Malaysia. Thank you for visiting!
Wednesday, December 8, 2010
The missed canal: hidden or neglected?

Monday, November 1, 2010
Peri-apical healing of a cracked tooth

 Tooth 25 had a vertical fracture line that extended from mesial marginal ridge and all the way down into the orifice of palatal canal. I thought this was a hopeless case and the patient was very keen to keep the tooth. After dressing with CaOH for two weeks, there was still exudation in palatal canal. Obturation was done after six weeks of CaOH and when both canals were dry. A six-month review showed evidence of peri-apical healing.
Tooth 25 had a vertical fracture line that extended from mesial marginal ridge and all the way down into the orifice of palatal canal. I thought this was a hopeless case and the patient was very keen to keep the tooth. After dressing with CaOH for two weeks, there was still exudation in palatal canal. Obturation was done after six weeks of CaOH and when both canals were dry. A six-month review showed evidence of peri-apical healing. 
Friday, October 29, 2010
Dealing with curved canals


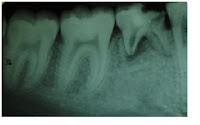
My siren started to ring when I saw a pre-op pa radiograph like this one here. My main concerns were not to ledge the canal, maintain patency and avoid separating instrument at the apical curve in the mesial root. This was my strategy. After establishing a glide path with #8 file, I straightened the coronal third of the canal. Making sure that patency was maintained, I precurved all hand files and enlarged it to #20. Subsequently, the canal was shaped with Profile 0.06 taper to to #30.
Tuesday, October 26, 2010
Retreatment


Each pulp is unique!
Tuesday, October 5, 2010
Latex-free Root Canal Treatment

Sunday, October 3, 2010
Unusual C-shaped canal



Thursday, September 30, 2010
Toothache or neuralgia?


Wednesday, September 29, 2010
Nice healing of a large peri-apical lesion


Friday, August 20, 2010
An extreme approach to an open root end
(This article is expected to be published in the Malaysian Dental Association (MDA) News)
Root canal treatment (RCT) on an immature permanent tooth with necrotic pulp and apical periodontitis remains a challenge to us, dental clinicians. Cases of traumatized immature upper incisors, immature lower premolars with fractured dens evaginatus and sometimes in deep caries lesions of immature first molars may lead to pulplal injuury and RCT. An immature tooth takes approximately three years after its eruption for apical closure. If the tooth is still in an early stage of root development, canal walls will be thin and fragile. The absence of an apical constriction poses challenges in standard cleaning and shaping procedures and it is difficult to obtain a good seal during obturation.
A procedure called apexification is currently the first line of treatment for immature necrotic permanent teeth (1). According to American Association of Endodontists Glossary of endodontic terms (2003), apexification is defined as a method of inducing a calcified barrier of a root with an open apex or continued apical development of an incomplete root in teeth with necrotic pulp. The canal is filled with calcium hydroxide (CaOH) to induce the formation of an apical hard tissue barrier, which composed of dentin, cementum, bone or osteodentin. This process usually took 6 to 18 months. Apexification with mineral trioxide (MTA) shortened the long duration of this mode of treatment to single or two visits and the aim was to provide an effective apical seal without any attempt for apical closure. Apexification, unlike apexogenesis, do not promote root lengthening and thickening of lateral walls. Therefore, immature teeth with thin canal wall are more susceptible to vertical fractures, either during or after apexification. Do you ever question if it is worthwhile saving immature teeth, especially those with thin walls, or replacing them with implants is a better option?
Apexogenesis refers to a vital pulp therapy procedure performed to encourage physiological development and formation of the root end, whereas apexification is only performed onto non-vital teeth. There are several clinical case reports that did not show a clear cut between these two clinical procedures. When an apexogenesis approach is performed on a non vital infected immature tooth, continued root development was observed (2). This stimulates new perceptive on how we treat immature teeth with necrotic pulp, favouring apexogenesis over apexification.
Revascularization is a new treatment protocol to generate tissues into pulp space of nonvital infected tooth (3). In order to create an environment for regeneration of infected necrotic teeth:
· Canal has to be effectively disinfected
· Matrix in the form of blood clot has to be created in the canal to allow new tissue to grow
· Coronal access has to be tightly sealed to prevent recontamination.
Banchs and Trope described the revascularization method of an immature necrotic permanent lower premolar with apical periodontitis and sinus tract (4). Infection was controlled by copious irrigation of sodium hypochlorite (NaOCl) and a triple antibiotic preparation, consisting of minocycline, ciprofloxacin and metronidazole, as the intra-canal medicament. No mechanical instrumentation was recommended as it might further weakened the root. When the canal was clean and free from inflammatory exudates, bleeding was intentionally created by irritating apical tissues gently, to form a blood clot below the cemento-enamel junction and the access cavity sealed with MTA and composite restoration. The tooth was asymptomatic, the sinus disappeared and radiolucency reduced in size after 26 days. Subsequent radiographic evaluation up to two years showed successful apexogenesis with root lengthening and lateral reinforcement of canal walls.
How does tissue regenerate and what is this new tissue in the pulp space? An immature open-apex tooth has a rich blood supply and contains stem cells with the capacity to regenerate. It is also possible that viable pulp cells at the apical part of the canal proliferate into the newly formed matrix. In the absence of intra-canal infection and presence of a matrix, these cells differentiate into odontoblast and deposit dentin, causing apexogenesis. Growth factors in the blood clot itself may also contribute to regeneration.
Revascularization is a new and promising topic in endodontics. In line with our general goal to preserve pulp vitality and conservative treatment, more research is looking into pulp regeneration for mature teeth. It is not impossible since there are vital pulp tissues in mature teeth with periradicular lesion and dental stem cells do exist on permanent teeth. In the era of stem cell technology, is pulp regeneration our new direction? RCT may be much simpler in future without mechanically instrumenting the intricate root canal system, instead, disinfection of the infected pulp and stimulation pulp regrowth will be the new protocol.
Having said all that, revascularization is still in its infancy as a routine endodontic procedure. There are still may uncertainties and we need more clinical studies to establish its guidelines and indications. We still do not know its long term outcome of this new procedure. Will there be mineralized tissues filling and obliterating the canal space and what is the impact of this occurrence? It will be a problem if the calcified canal is indicated for a conventional non-surgical RCT in future. For now, we can select cases carefully when attempting this new method. Duration of infection can be a determining factor. This can be worked out simply by checking the stage of root development on the periapical radiograph and age of the patient. Success will be less likely when an immature tooth has been necrotic and infected for more than five years. Gentle flushing of canal with NaOCl is cannot be overemphasized here to prevent injecting the solution into the soft tissues, which may cause a NaOCl accident. Minocycline, one of the three antibiotic mixture, should be used with caution in anterior teeth as it causes severe dentin staining. If there is no signs of regeneration after three months, the conventional method can be carried out.
If you would like to know more about revascularization and tissue regeneration, join us at the MES-SES Joint Meeting on 31st October, 2010. Two experts, Dr Jeeraphat Jantarat from Thailand and Dr Leung Siu Fai from Hong Kong, will share their clinical experiences and scientific knowledge in this topic. Hope to see you there.
References
1. Raftar M. Apexification: A Review. Dent Traumatol 2005; 21: 1-8
2. Chueh LH, Huang GT. Immature teeth with periradicular periodontitis or abscess undergoing apexogenesis: a paradigm shift. J Endod 2006; 32:1205-13
3. Iwaya S, Ikawa M, Kubota. Revascularization of an immature permanent tooth with apical periodontitis and sinus tract. Dent Traumatol 2001; 17:185-7
4. Banchs F, Trope M. Revascularization of Immature Permanent Teeth with apical periodontitis: New treatment protocol? J Endod 2004; 30 (4): 196-200
Monday, June 14, 2010
Implant or Root Canal?

Thursday, May 13, 2010
Root Canal Politics?

Monday, April 19, 2010
Tell me your pain...

Thursday, April 15, 2010
Thursday, April 1, 2010
Working with a Dental Dam

The rubber dam is easy to apply and it is usually placed at the beginning of root canal treatment after the local anaesthetic is administered. Patients who are allergic to rubber can opt for the latex-free dental dam.
Sunday, March 28, 2010
Missing teeth
There are also cases where the patients complain of toothache due to large decay on these teeth. Sometimes, I perform a root canal treament, provided the root are not resorbed, in order to keep the tooth functioning in the oral cavity for as long as possible, especially for a young patient. However, the prognosis maybe be guarded. It is also possible that the retained primary tooth is fused to the jaw bone (ankylosed). I supposed one will just have to accept the fact that he or she is born with less teeth and ultimately, will need dental implants.
Friday, March 26, 2010
My Friday morning routine

Thursday, March 25, 2010
X-ray Vision

Wednesday, March 24, 2010
Give Root Canal Treatment a Second Chance.
I was taught in my Masters programme that RCT has 70-90% of favourable treatment outcome. Perhaps this patient is one of the few unlucky ones. I will not bore you with the long list of reasons that influence the outcome of RCT, but I just want to emphasize here that if the treatment is carried out under acceptable standard of care, it will usually solve the patient's painful experience due to the dental infection. If the tooth is still restorable, RCT is definitely the better option than removing it. Losing your teeth will also lead to a set of other dental problems later on.
So, to these people who refuse RCT, don't let that just one bad experience influences your decision, give RCT a second chance!
It is also possible to retreat or repeat the RCT on a tooth when the first RCT does not have a favourable outcome.
